BRIAN HICKEY: Ever since a hit-and-run driver mowed me down in Collingswood on Nov. 28, I’ve been considered a “patient.” The conversational-English translation of that term is “dramatically injured person at the total mercy of insurance-company whims.” After I was released from inpatient care at Philadelphia’s Magee Rehabilitation in January, I was forced to wait more than six weeks for outpatient physical, occupational, and cognitive therapy. For context, more than two weeks of waiting risks regression on all three fronts.
My mistake? Figuring my local insurance company would grasp why I wanted to stick with the therapist who inexplicably got me back on my feet within three weeks of being in a coma. She did so, in part, by never letting me pull the too-tired card – even in the early days, when I was speechless and prone to brain-injury-related tantrums. As a 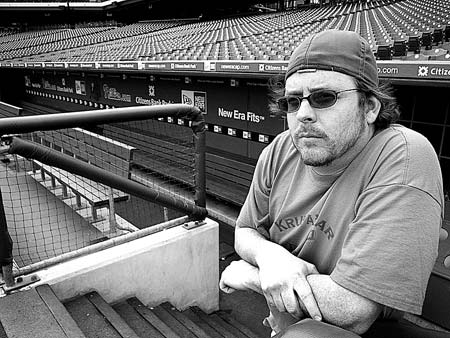 result of her motivational work and that of the whole rehab team, my mental and physical strength returned quicker than expected.
result of her motivational work and that of the whole rehab team, my mental and physical strength returned quicker than expected.
So continuing therapy at Magee was a no-brainer to my healing brain. But to the insurance company, it was a no-gainer. Despite having covered nearly seven expensive weeks of treatment, including a month of inpatient rehabilitation at Magee, my insurer sent me reams of legalese-laden letters to explain why it couldn’t let me go to Magee as an outpatient. Of particular interest was one that listed the wrong date for my injury and sold short my ability to walk properly, but at least got my last name correct. (Bravo!) The paraphrased summary: “You don’t know what’s best for you. You’ll adapt perfectly to your new designated provider. Oh, and here’s a bill. We’ll be covering $312.84 of the remaining $17,580 that saved your life at Cooper. Ciao!” MORE
